What Is It?
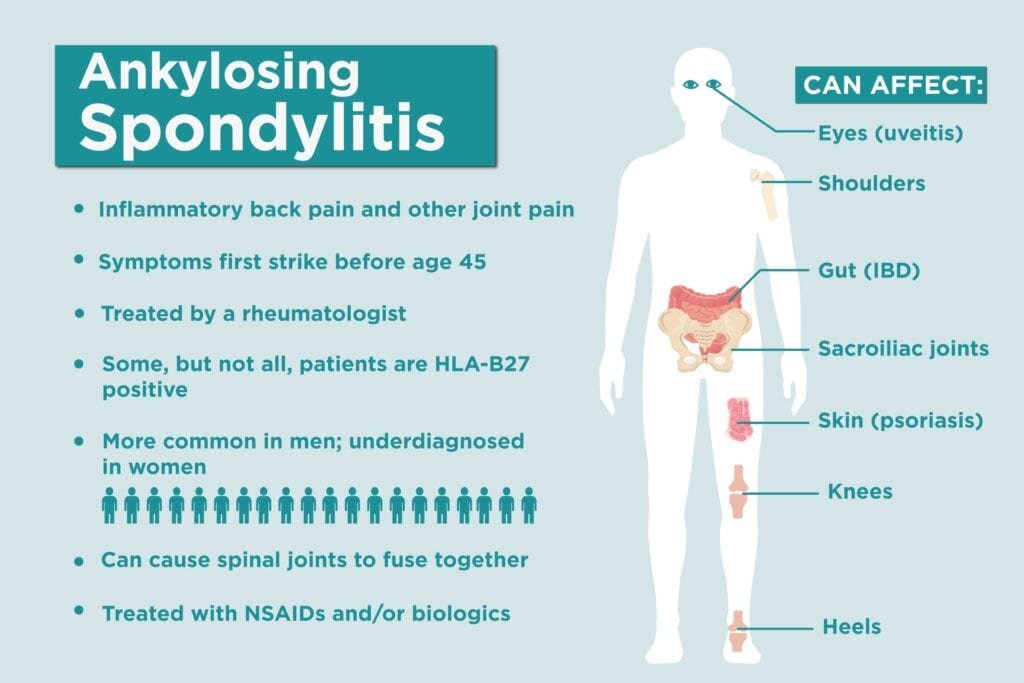
Ankylosing Spondylitis (AS) is a chronic auto-immune condition under the umbrella group of spondyloarthritis (SpA). It is a type of arthritis that causes inflammation primarily affecting the axial skeleton: the spine (cervical, thoracic and lumbar), sacroiliac joints, hips, shoulders and adjacent soft tissues.
Is It In The Genes?
There is still a lot to be learnt about the pathogenesis of ankylosing spondylitis, however we do know that there is a relation to your genes. One of the most important genetic factors is a class 1 allele HLA-B27. 90-95% of AS populations are HLA-B27 positive, however only 1-2% of HLA-B27 positive populations develop AS. This number increases to 15%–20% for those with an affected first-degree relative.
However, HLA-B27 positivity is not sufficient for diagnosis of AS as asymptomatic populations can also have the gene. The condition is also not directly passed from parent to child. Blood markers are useful in diagnosis and monitoring of disease progression, as well as treatment responses.
C-reactive proteins (CRP) and erythrocyte sedimentation rate (ESR) are the most common blood markers and are elevated in approximately 40-50% of AS patients. Once again, it is worth mentioning that these blood markers are not 100% indicative of AS, they must be considered along with the entire clinical presentation.
Clinical presentation
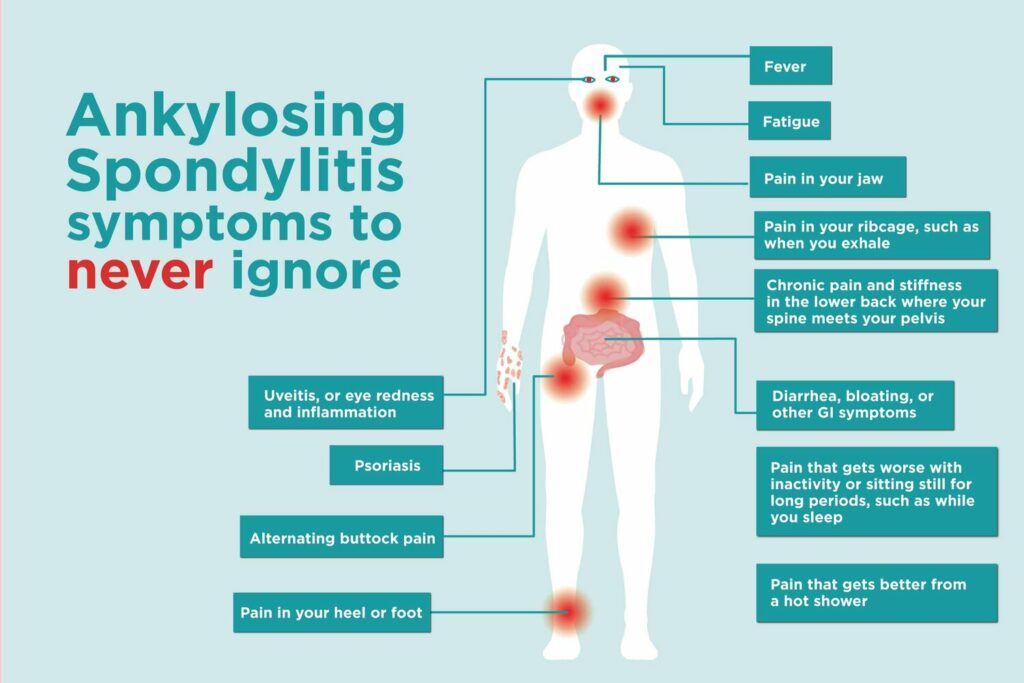
- Family history of spa.
- Chronic back pain (>3 months) onset prior to the age of 45.
- Early morning stiffness and/or pain lasting longer than 60-minutes. Eases throughout the day or with activity.
- Pain that wakes you up in the second half of the night.
- Extreme fatigue.
In addition, there are common extra-articular features and conditions related to ankylosing spondylitis including (prevalence);
- Enthesitis (40%)
- Peripheral arthropathy/synovitis (30%)
- Iritis/uveitis (20-26%)
- Crohns/ulcerative colitis (4-10%)
- Psoriasis (9%)
- Dactylitis (7%)
In more advanced cases of as the inflammation can lead to calcification and fibrosis (new bone formation) resulting in a loss of flexibility and fusion of the spine. The structural changes of the vertebrae have been likened to bamboo, due to the squaring and bridging of the vertebral bodies and decreasing disc space giving the visual appearance of bamboo on imaging.
There are further complications that can occur in individuals as a result of as. One is that of a higher risk of developing osteoporosis (low bone mineral density). Research here shows this to be due to the effects of systemic inflammation and reduced mobility. There is also evidence here as can slightly increase your risk of cardiovascular events by 30-50%, such as a heart attack or a stroke. Again this is largely due to the systemic inflammation of as. Which is why it is important to take antiinflammatory medication, exercise regularly, eat healthy and not smoke.
If you would like to learn more about the etiology, pathology and treatment please read the following papers here and here.

Diagnosis
Symptoms of ankylosing spondylitis can be similar to more common back pains and problems, especially in the early stages, making early diagnosis a challenge. It often starts in people during their late teens or twenties. Which is why many people put up with the pain for some time before seeking help, leading to an average delay of 8 years in diagnosis. It is important to see a healthcare professional as soon as possible if you suspect you have AS.
If suspected of AS you will usually be referred to and diagnosed by a Rheumatologist, who specialise in conditions affecting joints, bones and muscles. Diagnosis will be made based on several things, including;
- A history of your condition and the symptoms you have experienced
- Physical examination
- Blood tests – this is to confirm whether you have the HLA-B27 gene. Which may help diagnosis as there are links to this gene and AS, however it won’t confirm the diagnosis as people without the condition can also have the gene.
- X-rays or a magnetic resonance imaging (MRI) scan – x-ray remains the best for detection as it has greater sensitivity to new bone growth. An MRI can be useful in detecting signs of sacroiliitis (inflammation of the sacroiliac joints).

The goal of managing patients with AS is to maximise long-term health outcomes and help improve/maintain quality of life. Optimal management of AS requires a combination of pharmacological and non-pharmacological treatments.

Pharmacological Treatments
There are a range of medications used to help reduce pain and/or limit the effects of the condition.
- Non-Steroidal Anti-inflammatory Drugs (NSAIDs) like ibuprofen are used as an initial medication to help settle symptoms. They reduce pain, inflammation and disease activity.
- Disease Modifying Anti-Rheumatic Drugs (DMARDs) such as sulfasalazine and methotrexate, are more commonly used to treat other forms of arthritis and aren’t usually as effective in AS however they are prescribed in some cases. DMARDs aim to treat both the symptoms and prevent joint damage by reducing the amount of inflammation occurring in the body. They can take several weeks to months to take effect and are long-lasting treatments. When using DMARDs you will require regular check-ups and blood tests to monitor the effect.
- Newer emerging medication treatments in the form of biological therapies, called anti-tumour necrosis factor (TNF) medication that are shown to be very effective in people with AS. The following are used for AS; etanercept, adalimumab, certolizumab pegol and golimumab. These drugs have a more targeted approach to stop inflammation. They may not be suitable for everyone and are currently primarily prescribed to those whose condition cannot be controlled with the above mentioned drugs and physiotherapy.
- Another type of biological therapy is that of secukinumab. This is a newer therapy and is part of the interleukin (IL-17) inhibitors, which reduces or slows inflammation. These are in the form of injections that can be self administered. The effects of biological therapies are monitored to check how well they work.
If you would like to know more about the medications please read the paper HERE.

Physiotherapy
Physiotherapy is recommended to create and initiate an individualised exercise programme, with periodic reviews to assess changing needs. The aim of a physiotherapy programme is to:
- Improve physical function
- Decrease inflammation, joint damage and symptoms
- Decrease fatigue
- Reduce comorbidities
Research HERE has shown that physiotherapy programmes focusing on cardiorespiratory (cycling, running, walking) and strength exercises, have not only been shown to be safe but also have beneficial effects on disease activity in terms of inflammation, joint damage and symptoms. Greater effects are found in programmes that last longer than 12 weeks, so it is important to create an exercise routine that you can adhere to.
Previously, exercise interventions have mainly been focused on low to moderate exercises however in recent years numerous pieces of research, like HERE and HERE have identified high intensity training (HIT) as a safe and effective form of exercise (training in maximal heart rate values of 70-95%). Originally believed to exacerbate and aggravate symptoms, one research’s findings show that a 3 month programme of HIT resulted in no flare ups and to be as effective in disease modification as the TNFalpha-inhibitor. However, others have found the combination of anti-TNF treatment plus rehabilitation is more effective in terms of reducing symptom severity, improving functional and quality of life, activities of daily living and exercise parameters.

Ankylosing spondylitis is a progressive inflammatory arthritis, primarily affecting the spine and sacroiliac joints. The diagnosis of AS is complex involving a culmination of factors and requires a thorough investigation with the care of a Rheumatologist. The management follows a combination of pharmacological and non-pharmacological techniques. Physiotherapy management should include a regular exercise programme (in sessions and at home/gym) focussing on aerobic, resistance, neuro-muscular and flexibility exercises. To gain the best results those with AS need to fully adhere to their treatments and keep active.





